Gut Health, Well-Being, and More: The Essential Role of Serotonin in the Body
Serotonin, popularly known as the “happiness hormone,” is a fundamental…
Continue reading

It is estimated that between 57 and 65% of the world’s population suffers from lactose intolerance (1, 2), making it one of the main gastrointestinal problems today. Most people are born with the ability to digest lactose, which is the main carbohydrate in milk. However, many individuals lose this ability at some point in their lives.
For this reason, in this article, SYNLAB answers some of the main questions about the topic. Here you can read about:
Lactose is a disaccharide sugar found in mammalian milk, making up about 2% to 8% of milk, but this amount can vary between species and individuals (3).
Lactose is a large sugar molecule composed of two smaller sugar molecules, glucose and galactose. It is first broken down into glucose (used as an energy source) and later into galactose (a component of glycolipids and glycoproteins) by the enzyme lactase, to then be absorbed by intestinal enterocytes into the bloodstream (4).
The digestion and absorption of lactose occur in the small intestine.
Lactase activity can be detected on the surface of the intestinal mucosa from the eighth week of gestation, peaking in the 34th week. However, from the first month of life, it begins to decrease (lactase non-persistence), and its decline is highly variable from weaning to undetectable levels, as a normal consequence of the negative regulation of its activity (5).
In humans, about 30% of the population has continuous lactase activity after weaning into adulthood, thus enabling the consumption of large amounts of lactose (4).
The lactase enzyme is encoded by the LCT gene and is responsible for the hydrolysis (breakdown) of lactose into glucose and galactose (6). The control of the expression of the LCT gene is regulated by the MCM6 gene. Some individuals have variants in this gene that maintain the production of intestinal lactase, allowing these people to properly digest milk throughout their lives.
If the enzyme is absent (alactasia) or deficient (hypolactasia), the unabsorbed lactose molecules attract fluid into the intestinal lumen, leading to an increase in the volume and fluidity of the intestinal contents.
Additionally, unabsorbed lactose passes into the colon, where it is fermented by bacteria that produce short-chain fatty acids and gases, possibly causing various gastrointestinal symptoms (7).
It is a gastrointestinal condition characterized by the inability of an individual to digest lactose, a sugar present in milk and dairy products, usually caused by the deficiency of the enzyme lactase (8).
Hypolactasia, or lactase deficiency, is the “failure” in the expression of the lactase enzyme in the small intestine (9). This results in a condition that leads to poor lactose absorption, generally occurring after 6 to 7 years of age, and may arise later, with a steady increase in the prevalence of this condition, even in people over 65 years old (10).
The process of reduction and the amount of residual lactase have considerable variability among different ethnic groups and even among individuals. However, 50% of the lactase enzyme is sufficient to ensure effective lactose digestion (11).
The existing types of lactose intolerance are:
Congenital intolerance is an autosomal recessive condition where the child has genetic variants in both copies of the LCT gene. It is characterized by severe diarrhea from the first milk ingestion, preventing breastfeeding (only lactose-free formulas can be used). This condition persists throughout life and requires the complete exclusion of lactose sources (3).
This form of lactose intolerance is extremely rare. The nutrient deficiency causes growth delay, with rapid onset of dehydration and alkalosis.
Primary intolerance (lactase non-persistence) results from the physiological decline of lactase activity in intestinal cells and affects a large part of the population.
It is a known cause of abdominal discomforts such as diarrhea, abdominal distension, and flatulence. Its incidence shows great variability among ethnicities (12).
Lactase non-persistence is a normal condition represented by the loss of lactase expression and is associated with a point variant in the LCT gene, where the nitrogenous base cytosine is replaced by thymine (C>T) (3).
The CC genotype is associated with hypolactasia (residual lactase is approximately 10% compared to birth levels), while the TT genotype is associated with persistent lactase activity. The presence of a CT genotype predisposes to intermediate levels of lactase expression (13).
Secondary intolerance occurs when damage to the intestinal mucosa causes a temporary lactase deficiency (14).
Typically, small intestine diseases can cause secondary lactase deficiency, such as:
However, bacterial, viral, or parasitic infections are more common, such as giardiasis, which induces transient enzyme loss in the mucosa affected by the inflammatory or infectious process.
This is a reversible condition that requires a lactose-free diet until normal intestinal mucosa is restored (15).
Lactose malabsorption refers to any cause of failure to digest and/or absorb lactose in the small intestine and is a necessary precondition for lactose intolerance (16).
However, the two should not be confused, as many individuals with malabsorption do not show symptoms after consuming dairy products.

The symptoms of lactose intolerance, as well as their severity, can vary among individuals, depending on the amount of lactose ingested and the individual’s ability to digest it. The onset of these symptoms is strongly related to the appearance of hydrogen gas during breath tests. The most common intestinal symptoms include (17):
Some studies have reported that the clinical presentation of lactose intolerance is not limited to intestinal complications (18). Around 20% of individuals may experience cardiac arrhythmia and some neurological symptoms such as:
One of the possible factors responsible for these systemic effects may be the production of toxic metabolites generated by lactose fermentation in colon bacteria, which can alter cellular signaling mechanisms.
When systemic complaints are present, it is important to rule out cow’s milk protein allergy, which occurs in up to 20% of patients with clinical conditions of lactose intolerance (19).
Gastrointestinal symptoms of intolerance can resemble cow’s milk allergy and may be incorrectly labeled as “milk allergy” symptoms, leading to misdiagnosis and improper dietary management (20).
The treatment of lactose intolerance involves reducing, but not completely eliminating, foods that contain lactose (21).
On the other hand, individuals suspected of cow’s milk protein allergy should undergo a restricted diet test with elimination of cow’s milk protein-based foods.
There are significant differences between lactose intolerance and cow’s milk allergy; therefore, a better understanding of these differences could limit misunderstandings in the diagnostic approach and management of these conditions.
Several tests can be performed for this diagnosis, with the most common ones being (22-24):
This is the preferred method for evaluating lactose malabsorption and intolerance. It assesses abnormal hydrogen excretion in exhaled air after ingestion of a standard dose of lactose (diluted in water). Since hydrogen is not produced by mammalian enzymes, its presence indicates sugar contact with bacteria, indicating malabsorption.
This test evaluates the increase in blood sugar at different times (e.g., 30, 60, and 120 minutes) after ingestion of 50g of lactose.
The gaxilose test involves administering lactase substrate gaxilose (4-galactosylxylitol) with evaluation of D-xylitol in urine or blood. Gaxilose measurement is ideal for assessing intestinal lactase, as enzyme activity is evaluated throughout the small intestine.
Evaluates the presence of variants in genes associated with intolerance. However, it is not suitable for secondary lactase deficiency.
The main limitation of genetic, enzymatic and gaxilose tests is that malabsorption is common in healthy individuals, and a positive result does not confirm that symptoms are caused by this condition. Generally, the hydrogen breath test is the method of choice as it provides reasonably reliable information about digestive function and patient symptoms.
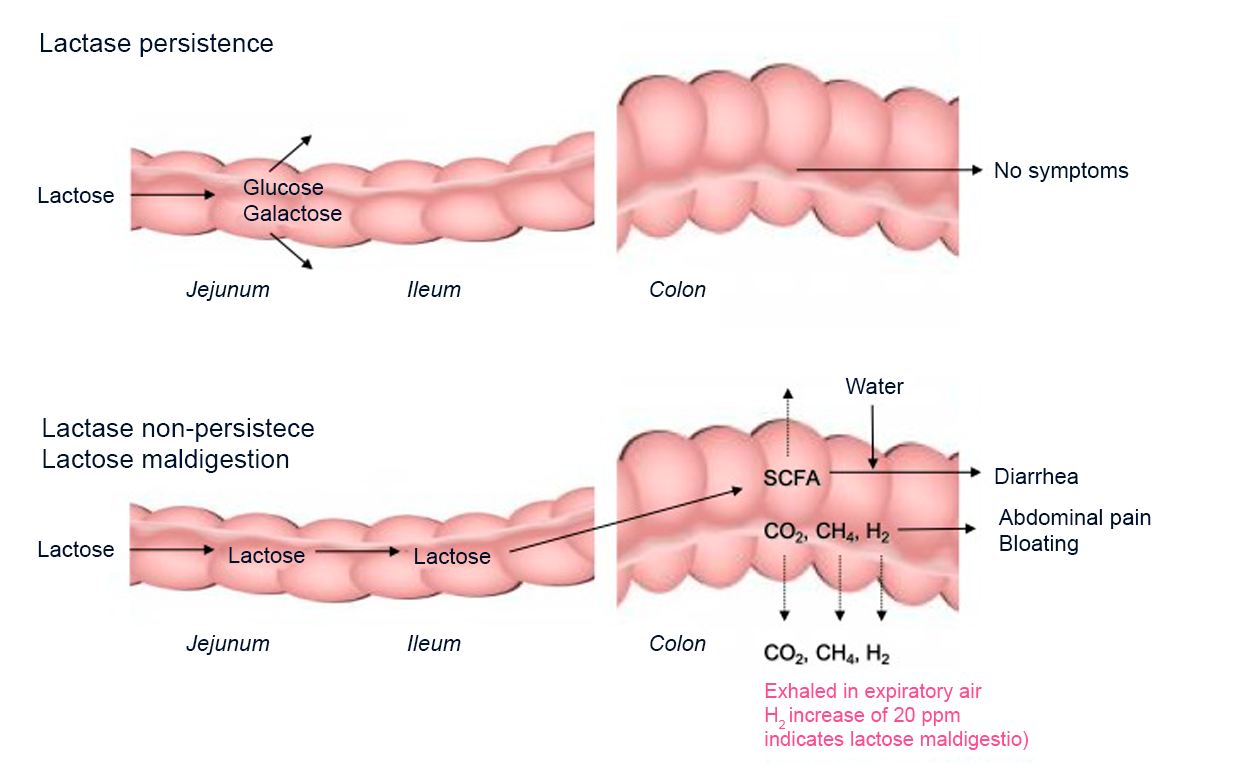
The process of lactose digestion in patients with lactase persistence and deficiency illustrating the relationship between lactose malabsorption, visceral sensitivity, and symptoms
Modified from Misselwitz et al, 2019(24)
Conducting precise tests is essential for making more accurate diagnoses. SYNLAB offers the following tests:
The Lactose Test involves the genetic analysis of the patient’s DNA to determine the presence of the main variants (-13910C/T and -22018G/A) in the MCM6 gene, which are associated with the development of lactose intolerance in adulthood.
The test is performed using the Sanger Sequencing technique, which determines the exact sequence in which the nucleotides are found in the MCM6 gene for the studied variants.
It is indicated for:
The INTOLERANCE2 test allows you to know in a single analysis if there is a genetic predisposition to celiac disease and/or primary lactose intolerance. As an alternative to the breath test, the analysis is performed from a blood sample, avoiding the patient’s direct exposure to substances.
It is indicated for:
The SYNLAB Hydrogen Test detects the condition through gas chromatography analysis.
Once lactose intolerance is diagnosed, the doctor may recommend a low-lactose diet to improve symptoms and avoid the long-term risk of malnutrition.
However, in the presence of symptoms and inconclusive diagnostic investigations, a detailed diet along with a symptom history should be performed, and if appropriate, lactose-containing foods can be excluded from the diet until symptoms improve (usually for at least four weeks).
Nutritional counseling should be sought to ensure diet adequacy.
Precise and up-to-date tests are essential for more accurate diagnoses and better treatment guidance. SYNLAB is here to help you.
We offer diagnostic solutions with strict quality control for the companies, patients, and doctors we serve. We have been in Brazil for over 10 years, operate in 36 countries and three continents, and are leaders in service provision in Europe.
Contact the SYNLAB team and learn about our tests.
1. Catanzaro R, Sciuto M, Singh B, Pathak S, Marotta F. Irritable Bowel Syndrome and lactose intolerance: the importance of differential diagnosis. A monocentric study. Minerva Gastroenterol (Torino), 67 (1) (2021), pp. 72-78, 10.23736/S1121-421X.20.02734-8.
2. Storhaug CL, Fosse SK, Fadnes LT. Country, regional, and global estimates for lactose malabsorption in adults: a systematic review and meta-analysis Lancet Gastroenterol Hepatol, 2 (2017), pp. 738-746, 10.1016/S2468-1253(17)30154-1.
3. Di Rienzo T, D’Angelo G, D’Aversa F, Campanale MC, Cesario V, Montalto M, Gasbarrini A, Ojetti V. Lactose intolerance: from diagnosis to correct management. Eur Rev Med Pharmacol Sci. 2013;17 Suppl 2:18-25.
4. Lomer MC, Parkes GC, Sanderson JD. Review article: lactose intolerance in clinical practice–myths and realities. Aliment Pharmacol Ther. 2008 Jan 15;27(2):93-103.
5. Matthews SB, Waud JP, Roberts AG, Campbell AK.Systemic lactose intolerance: a new perspective on an old problem. Postgrad Med J. 2005 Mar;81(953):167-73.
6. Campbell AK, Waud JP, Matthews SB. The molecular basis of lactose intolerance. Sci Prog. 2005;88(Pt 3):157-202.
7. Spohr A, Guilford WG, Haslett SJ, Vibe-Petersen G. Use of breath hydrogen testing to detect experimentally induced disaccharide malabsorption in healthy adult dogs. Am J Vet Res. 1999 Jul;60(7):836-40.
8. Heine RG, AlRefaee F, Bachina P, De Leon JC, Geng L, Gong S, Madrazo JA, Ngamphaiboon J, Ong C, Rogacion JM. Lactose intolerance and gastrointestinal cow’s milk allergy in infants and children – common misconceptions revisited. World Allergy Organ J. 2017 Dec 12;10(1):41.
9. Seppo L, Tuure T, Korpela R, Järvelä I, Rasinperä H, Sahi T. Can primary hypolactasia manifest itself after the age of 20 years? A two-decade follow-up study. Scand J Gastroenterol. 2008;43(9):1082-7.
10. Di Stefano M, Veneto G, Malservisi S, Strocchi A, Corazza GR. Lactose malabsorption and intolerance in the elderly. Scand J Gastroenterol. 2001 Dec;36(12):1274-8.
11. Swallow DM. Genetics of lactase persistence and lactose intolerance. Annu Rev Genet. 2003;37:197-219.
12. De Ritis F, Balestrieri GG, Ruggiero G, Filosa E, Auricchio S. High frequency of lactase activity deficiency in small bowel of adults in the Neapolitan área. Enzymol Biol Clin (Basel). 1970;11(3):263-7.
13. Enattah NS, Sahi T, Savilahti E, Terwilliger JD, Peltonen L, Järvelä I. Identification of a variant associated with adult-type hypolactasia. Nat Genet. 2002 Feb;30(2):233-7. doi: 10.1038/ng826.
14. Vesa TH, Marteau P, Korpela R. Lactose intolerance. Review J Am Coll Nutr. 2000 Apr;19(2 Suppl):165S-175S.
15. Usai-Satta P, Scarpa M, Oppia F, Cabras F. Lactose malabsorption and intolerance: What should be the best clinical management? World J Gastrointest Pharmacol Ther. 2012 Jun 6;3(3):29-33.
16. Misselwitz B, Butter M, Verbeke K, Fox MR. Update on lactose malabsorption and intolerance: pathogenesis, diagnosis and clinical management. Gut. 2019 Nov;68(11):2080-2091.
17. Zhao J, Fox M, Cong Y, Chu H, Shang Y, Fried M, Dai N. Lactose intolerance in patients with chronic functional diarrhoea: the role of small intestinal bacterial overgrowth. Aliment Pharmacol Ther. 2010 Apr;31(8):892-900.
18. Harrington LK, Mayberry JF. A re-appraisal of lactose intolerance. Int J Clin Pract. 2008 Oct;62(10):1541-6.
19. Campbell AK, Matthews SB, Vassel N, Cox CD, Naseem R, Chaichi J, et al. Bacterial metabolic ‘toxins’: a new mechanism for lactose and food intolerance, and irritable bowel syndrome. Toxicology. 2010 Dec 30;278(3):268-76.
20. Heine RG, AlRefaee F, Bachina P, De Leon JC, et al. Lactose intolerance and gastrointestinal cow’s milk allergy in infants and children – common misconceptions revisited. World Allergy Organ J. 2017 Dec 12;10(1):41.
21. Yang J, Deng Y, Chu H, Cong Y, Zhao J, et al. Prevalence and presentation of lactose intolerance and effects on dairy product intake in healthy subjects and patients with irritable bowel syndrome. Clin Gastroenterol Hepatol. 2013 Mar;11(3):262-268.e1.
22. Rezaie A, Buresi M, Lembo A, Lin H, McCallum R, Rao S, et al. Hydrogen and Methane-Based Breath Testing in Gastrointestinal Disorders: The North American Consensus. Am J Gastroenterol. 2017 May;112(5):775-784.
23. Domínguez Jiménez JL, Suárez AF. Correlation Between Capillary and Venous Blood Glucose in the Lactose Tolerance Test. Dig Dis Sci. 2016 Jan;61(1):208-14.
24. Misselwitz B, Butter M, Verbeke K, Fox MR. Update on lactose malabsorption and intolerance: pathogenesis, diagnosis and clinical management. Gut. 2019 Nov;68(11):2080-2091.
Serotonin, popularly known as the “happiness hormone,” is a fundamental…
Continue reading
Have you ever felt discomfort after eating certain foods, such…
Continue reading
Dermatomyositis is a rare inflammatory disease that affects the skin…
Continue reading